Hospitals Avoid Catastrophic Emergencies with Advanced Backup Power Systems
To avoid the human toll and financial cost of extended power outages, many healthcare facilities are choosing to go beyond minimum standards with advanced emergency backup power infrastructure.
With thin financial margins common across healthcare systems, beyond-code emergency preparedness upgrades were once considered luxuries. But the importance of backup systems can no longer be ignored.
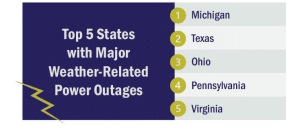
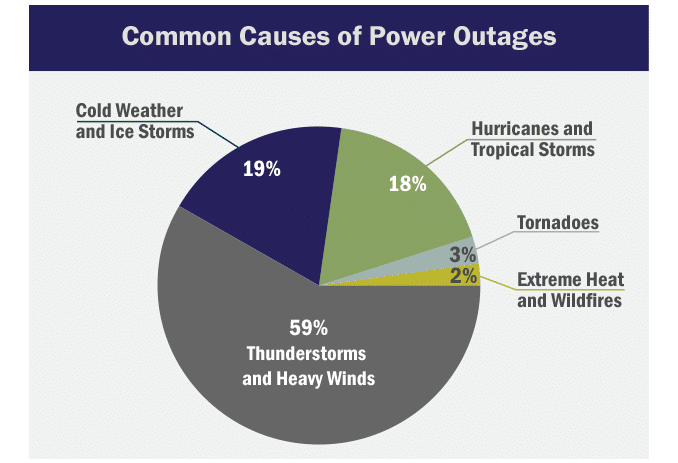
Extreme weather is increasing the frequency and intensity of blackout events. Combined with recent advances in power supply and distribution technologies, more hospitals are expanding renovations or updating master plans to develop more resilient, redundant and resource-efficient emergency power systems.
Recent utility data suggests the average number of annual weather-related power outages have at least doubled in recent years.
Losing Power Comes at High Cost
Recent utility data suggests the average number of annual weather-related power outages have at least doubled in recent years.
Source: Climate Central
It remains unusual for extended power outages to occur outside of a major weather event. Such incidents are, however, not unheard of. Reasons backup generators may stop working include:
- Age: Many generators were installed more than 50 years ago, beyond their useful lifetime.
- Flooding: Generators and fuel supplies are typically stored in flood-prone basements.
- Water Damage: Fuel stored in underground tanks risk contamination from prolonged exposure to damp conditions.
The likelihood of an outage may be rare. But the damage from a single event can be significant.
Across the industry, power outage disruptions cost healthcare facilities on average $60,000 per year, according to a survey by consultancy E Source. Actual costs can reach 4 percent of annual revenue.
Source: Climate Central
Understanding Emergency Power Requirements
Hurricanes and other recent disasters have led federal, state and local agencies to adopt more stringent emergency preparedness requirements.
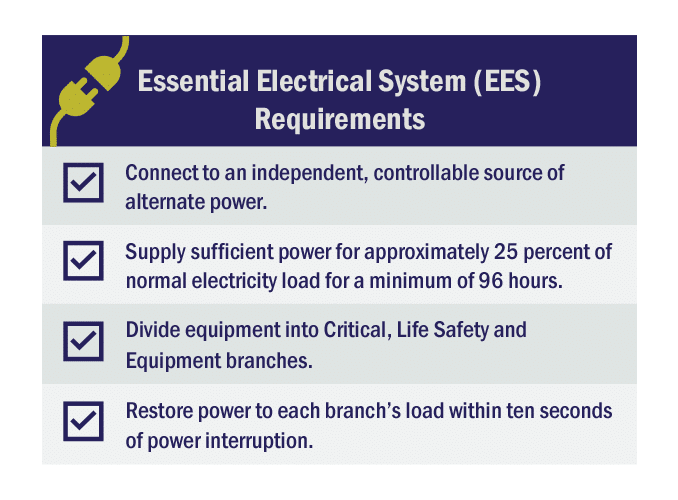
The Centers for Medicare & Medicaid Services (CMS), National Fire Protection Association (NFPA) and the Facility Guidelines Institute (FGI Guidelines) set criteria for healthcare facility emergency backup power, which many state and local authorities then adopt as part of their respective codes.
The result is a complex and evolving set of rules and standards for the design, operation, maintenance and performance capabilities of emergency power systems. Requirements vary by location and type of facility.
Healthcare facility codes only set minimum requirements. These are far from design guidelines. Instead, each facility and their team of consultants must design emergency preparedness systems that offer adequate resiliency based on currently foreseen conditions.
Adding Redundancy to Essential Electrical Systems
Hospital renovation plans are adding redundancy measures into Essential Electrical System designs.
Instead of relying on a single generator, facilities that install separate, paralleled generator systems can minimize risk of a blackout. Hospitals that choose not to dedicate scarce real estate for additional equipment and fuel can instead install an outdoor connection.
Hospitals that choose not to dedicate scarce real estate for additional generators and fuel can instead install an outdoor connection.
Also known as a “tap box” or “docking station,” the Generator Connection Cabinet enables hospitals to quickly and conveniently connect a portable generator to the electrical power distribution system in the event of the main generator failure.
During a power outage, electricity transfers automatically to the generator, but it can typically take up to 10 seconds for the load to reach proper voltage and frequency. For this reason, digitized medical equipment can take several minutes to boot up.
Uninterruptible Power Supplies (UPS) maintain continuous operation during this downtime. Adding extra UPS modules can ensure hospitals maintain critical loads without relying on the performance of a single unit.
When deploying an additional UPS, hospitals must then decide between a centralized or distributed system. A centralized UPS often comes with greater reliability but higher upfront costs. A distributed system, however, involves additional maintenance associated with frequently testing UPS batteries across the hospital, as required by code.
Other considerations include installing backup transfer switches and electric panels. As always, redundancy measures will be limited by the costs to design and to install the electrical system as well as the extent that construction would disrupt daily operations.
Empowering Healthcare with Distributed Energy Resources
For many years, a diesel generator was the only source of backup power that could comply with code.
Regulators are increasingly accommodating advanced power generation technologies that can be used to bolster emergency power capabilities. An increasing number of hospitals are able to avoid reliance on the grid altogether.
Cogeneration is the most common approach. Combined heat power (CHP) systems burn natural gas or biomass to generate electric power on site, using captured waste energy to meet the facility’s thermal needs.
Although the technology has been available for decades, about 20 percent of healthcare CHP systems came online in just the last five years.
Some hospitals are going one step further with the deployment of microgrids. The decentralized energy system relies upon CHP systems or other distributed energy resources, combined with battery storage technologies, to operate independently during an extended outage. Some can produce self-sustaining power all year round.
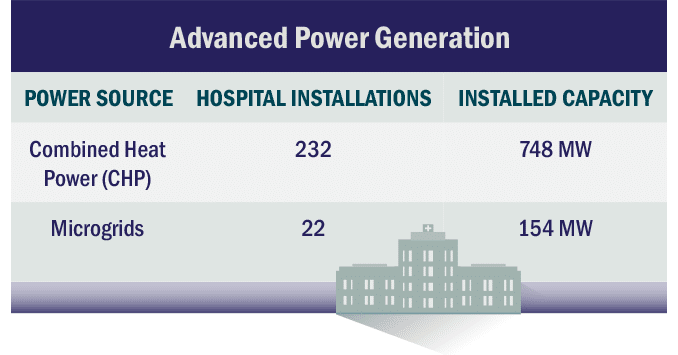
Source: U.S. Department of Energy
Distributed energy resources offer benefits even when the power is on. Tapping electricity stored in large-scale battery systems can improve the financial health of hospital operations, yielding savings at times of high electricity prices or to minimize peak demand charges.
Advanced power generation and battery storage systems also produce environmental benefits. Whereas traditional diesel-fed generators release harmful air contaminants, switching to energy-efficient sources can reduce on-site pollution and greenhouse gas emissions.
Preparing for the Future
Hospitals are allocating greater resources to resiliency, underscoring its importance.
Although neither generators, EES upgrades nor advanced power systems are reimbursable by Medicare or Medicaid, the business case for hospitals to dedicate operational funds toward emergency power preparedness is increasingly apparent as extreme weather becomes the norm.
Hospital leaders who exceed code requirements to proactively invest in resilient emergency power system are accepting new realities of an uncertain future. While the upfront cost of major system overhauls may be financially painful, each upgrade comes with the potential to improve quality of care and to save the lives of vulnerable patients.


