How Operating Room Designs Avoid the Shock of Electrical Accidents
During a routine arthroscopic shoulder repair, an operating table’s electrical panel short circuited, causing the table to suddenly decline. The surgical team swiftly moved the anaesthetized patient to a transport trolley before concluding the procedure, avoiding a potentially catastrophic outcome.
All this happened while intravenous fluid was leaking onto the floor. Despite mopping and suctioning, the surgical team stood over a wet film of water — a truly hazardous situation.
Electrical accidents within operating rooms are rare. Still, this incident — documented recently in the Journal of Anesthesiology Clinical Pharmacology — demonstrates why electrical precautions must remain ever-present concerns.
As operating room environments become increasingly complex and surgical teams rely more on sensitive electrical equipment, close collaboration between clinical staff and healthcare engineers can avoid the inherent hazards that electronic equipment pose to patients and staff.
Electrical Designs Account for Operating Room Complexity
Operating rooms feature a wide range of medical equipment requiring special design attention due to their reliance on complex electrical distribution systems.
Surgical teams directly handle electrical equipment and apply electrical devices to patients, making the design and function of electrical systems critical for operating room safety. Yet electrical safety protections vary considerably across the country’s operating rooms. Their design depends, in large part, on whether the procedures occurring in each space involve large amounts of fluids.
An unrestrained ground fault can result in severe electrocution, fire, explosions, or equipment damage
NFPA99: Healthcare Facilities Code requires special protection against electrical shock in facilities designated as “wet procedure locations.” This generally applies to clinical spaces where surgical procedures result in standing pools of liquid — from hospital environmental services notwithstanding — or spaces where future surgeries may result in standing fluids.
Wet Operating Room Requirements
NFPA 99 requires that wet procedure locations install either an ungrounded Isolated Power System (IPS) or Ground-Fault Circuit Interrupters (GFCIs).
The IPS is the preferred protection for essential electrical system (EES) circuits supplying wet procedure locations. GFCI protection, on the other hand, is not recommended on any critical load that cannot sustain an interruption of power. Doing so would risk unexpectedly shutting off critical devices such as life-support equipment.
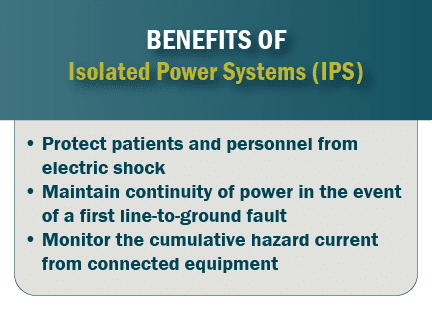
If a branch circuit’s phase conductor were to experience a phase-to-ground fault condition, the IPS allows for the operating room’s machinery to stay powered on.
An IPS not only minimizes potential for arcing, sparking, and fault currents to ignite an explosion or fire. The IPS can also reduce shock hazards from the inadvertent contact with a phase conductor.
To satisfy inspections, the IPS must be installed in accordance with specific branch-circuit conductor specifications. XHHW or XHHW-2 are the preferred conductors — not THHN/THWN. The installed conductors should follow particular color and striping requirements: orange for conductor No. 1, brown for No. 2, and yellow for No. 3. Stripes should use colors other than white, gray or green.
Monitoring Wet Operating Room Safety
A line isolation monitor continually monitors leakage and fault currents to ground, detecting resistance and capacitance at thresholds like that of high-impedance grounded neutral systems.
During a fault, rather than cut off power, the line isolation monitor sets off an alarm that notifies clinical staff of the ground fault. The line monitor would trigger an alarm for any fault hazard greater than 3.7 milliamp (mA) or for a total hazard current greater than 5 mA.
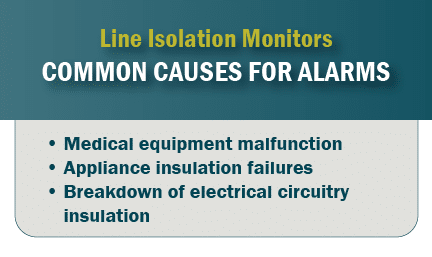 Upon hearing the alarm, medical personnel can exercise judgment on whether the threat of electrical shock requires an immediate response. Staff may choose, for example, to power down a defective piece of medical equipment.
Upon hearing the alarm, medical personnel can exercise judgment on whether the threat of electrical shock requires an immediate response. Staff may choose, for example, to power down a defective piece of medical equipment.
Recent advances in isolation monitor technology offer hospitals the option of troubleshooting a specific branch circuit. These insulation fault locator systems work directly with a line isolation monitor to locate the problematic circuit, significantly reducing the time involved in resolving a hazardous condition.
Wet Room Designations Are Open to Interpretation
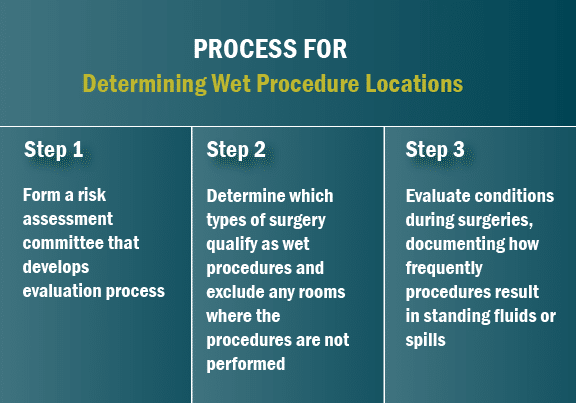
NFPA 99 classifies operating rooms as wet locations by default. That said, a facility’s surgical procedures may not necessarily result in any standing fluids — or fluids may be thoroughly addressed through mitigation factors such as irrigation techniques, mats, and table drains. In such circumstances, health care facilities can undertake risk assessments to determine whether each location is, in fact, more appropriately classified as a dry location.
 Each healthcare facility is empowered to reach a designation decision that makes most sense for its unique circumstances. Some hospitals choose to designate an operating room as a dry location to reduce design, construction and maintenance costs. Whereas other hospitals choose to designate their entire operating suite as wet procedure locations, creating a design uniformity that allows any surgery to be scheduled in any operating room. Such an approach is potentially more future proofed; as surgical procedures change over time, the hospital’s electrical distribution system would already comply with NFPA 99 requirements.
Each healthcare facility is empowered to reach a designation decision that makes most sense for its unique circumstances. Some hospitals choose to designate an operating room as a dry location to reduce design, construction and maintenance costs. Whereas other hospitals choose to designate their entire operating suite as wet procedure locations, creating a design uniformity that allows any surgery to be scheduled in any operating room. Such an approach is potentially more future proofed; as surgical procedures change over time, the hospital’s electrical distribution system would already comply with NFPA 99 requirements.
The risk assessment process involves input from clinicians, biomedical engineering staff, and facility safety engineering staff. With their input, the assessment considers:
- Types of procedures conducted at the facility — now and in the future
- Specific electrical equipment deployed within each operating room
- Various facility-specific procedures such as liquid mitigation protocols
Risk assessments should be undertaken with extreme caution. After all, it is the safety of patients and clinical staff — not budget or the nuisance of an alarm — that should form the basis of design.
Recognizing the additional cost of IPS installations, healthcare facilities can typically collaborate with inspectors and their authorities having jurisdiction (AHJs) to determine a long-term electrical system transition plan, gradually integrating new infrastructure into their facilities.
Education Key to Operating Room Designations
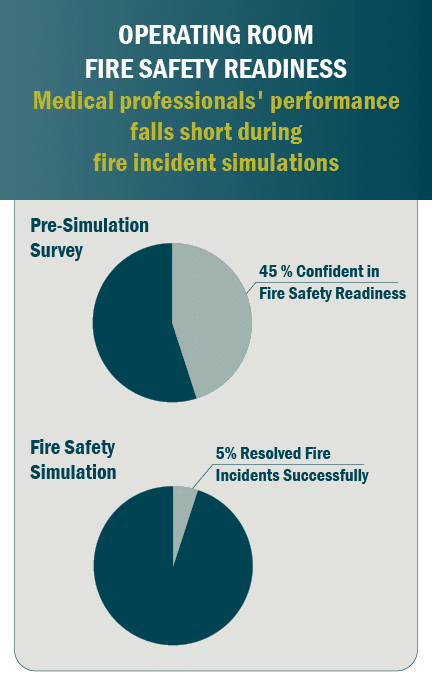
A lot is at stake when deciding whether to designate an operating room as a wet or dry procedure location. Unfortunately, general understanding among clinical staff about inherent electrical hazards remains relatively low.
Devices such as the IPS need to be installed correctly and tested frequently. Equally as important, medical personnel need to be trained and qualified on the proper use of sensitive electrical equipment such as the line isolation monitor.
A frequent complaint with line isolation monitors is that the operating room is already a noisy place. Medical alarms can sound off, on average, every minute during certain surgical procedures, according to a study published in Critical Care. Line isolation monitor alarms become yet another source of distraction.
Operating room sound levels frequently reach 70 dB(A) — equivalent to the hum of a vacuum cleaner
That said, the isolation monitor is not meant to be a nuisance. It is meant to protect lives. Unfortunately, many surgeons decide to minimize distractions by simply inactivating the alarm or altering the monitor activation settings.
Such decisions reflect a lack of training. Standard surgical textbooks provide scant details on causes of electrical accidents. Most surgical teams rely on the advice of sales representatives or industry-sponsored courses, and yet available trainings lack standardization. As a result, clinicians too often fail to comprehensively evaluate the consequence of their assessment decisions or misunderstand the significance of isolation monitor notifications.
Healthcare providers should turn to their healthcare engineering services consultant for guidance throughout the risk assessment process and for advice on operating equipment such as their IPS. Through close collaboration between electrical designers and clinicians, providers can strike a balance in their operating room designs: upholding the safety of patients and personnel, while accommodating the practical challenges of increasingly complex surgical facilities.
This article originally appeared in Consulting Specifying Engineer.