Innovative Operating Room Designs Limit Hospital Acquired Infections
Across the country, innovative mechanical system designs are exceeding code minimums to protect patients and healthcare workers from airborne infections.
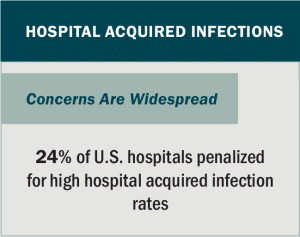
Operating rooms present a unique set of challenges. While efforts to limit hospital-acquired infections (HAI) are a priority throughout the hospital environment, operating rooms can be particularly concerning due to the proximity of surgical staff with immunocompromised or actively infectious patients.
In response, healthcare facilities are evaluating the most cost-effective approaches to provide safe surgical environments. Retrofitting and reconfiguring operating rooms to limit risks of indoor contamination will require collaborative approaches, combining new and established technologies with creative system designs.
Risks of Surgical Site Infections
Source: Centers for Medicare & Medicaid Services
Despite recent medical advances, the risk of contracting an infection while undergoing surgery remains disproportionately high.
Surgical site infection (SSI) is the leading cause of post-operative hospital readmission. Throughout surgical procedures, airborne particles carry microorganisms that can settle on surgical instruments or circulate throughout the operating room.
Microorganisms transmitted by textile fibers, dust particles, skin fragments, or respiratory aerosols infect an estimated 2-4 percent of patients undergoing inpatient surgical procedures.
Operating Room Code Requirements
Mechanical systems are fundamental to promote asepsis — the absence of dangerous bacteria, viruses and other microorganisms — and to maintain a sterile field in areas where surgeries are performed. Heating, ventilation, and air conditioning (HVAC) systems introduce fresh air, control relative humidity (RH) levels, and remove airborne contaminants.
In general, hospital HVAC system designs strive to continuously move air from “clean areas” such as an operating room to less-clean areas such as corridors or waiting areas. This is accomplished by keeping the sterile areas positively pressured and by controlling the directional path of airflow.
Source: The Lancet
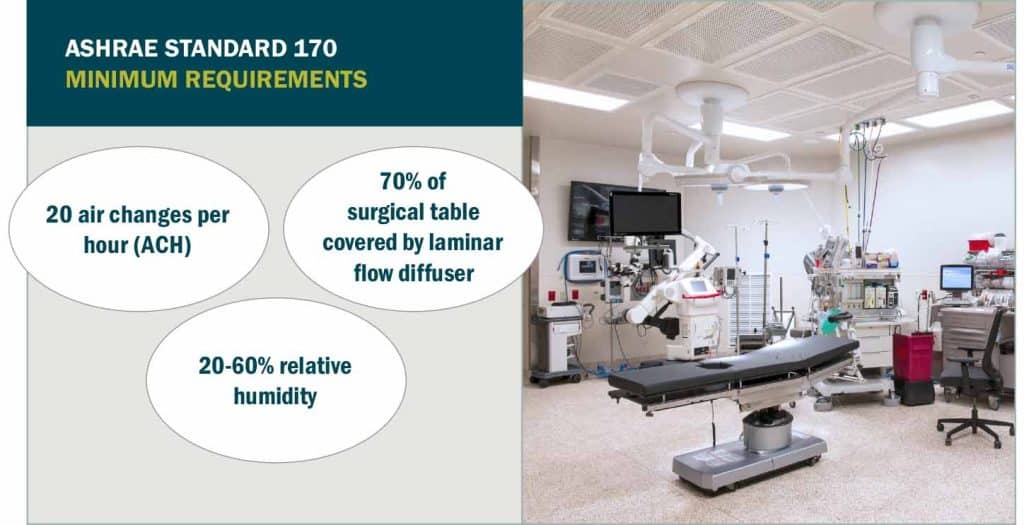
Requirements for healthcare mechanical system designs are based on American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) Standard 170. In recent years, Facility Guidelines Institute (FGI) coordinated with ASHRAE to incorporate Standard 170 within the FGI Guidelines.
Widely accepted by the healthcare industry and jurisdictional authorities, the standard sets effective levels for air change rates, ventilation rates, pressure relationships, redundancy measures, and other system design requirements.
Still, some hospitals and design engineers have realized the need to exceed code-minimum designs in an effort to further reduce infections and to improve quality of care. Beyond-code mechanical designs may involve:
- Raising minimum relative humidity levels,
- Increasing air exchange rates,
- Expanding distribution of laminar flow diffusers,
- Installing negative pressured isolation spaces, and
- Introducing air-filtration devices and ultraviolet-based pathogen inactivation systems.
Controlling Relative Humidity Levels
Humidification and temperature settings play uniquely important roles in limiting hospital infections.
A common misconception is that lower temperatures help control infection risks. In truth, operating rooms are kept cold for the comfort of robed surgical staff, wearing layers of personal protective equipment.
As temperatures decrease to achieve the surgical staff’s preferred comfort levels, RH levels increase. ASHRAE Standard 170 specifies indoor air levels stay between 20-60 percent RH.
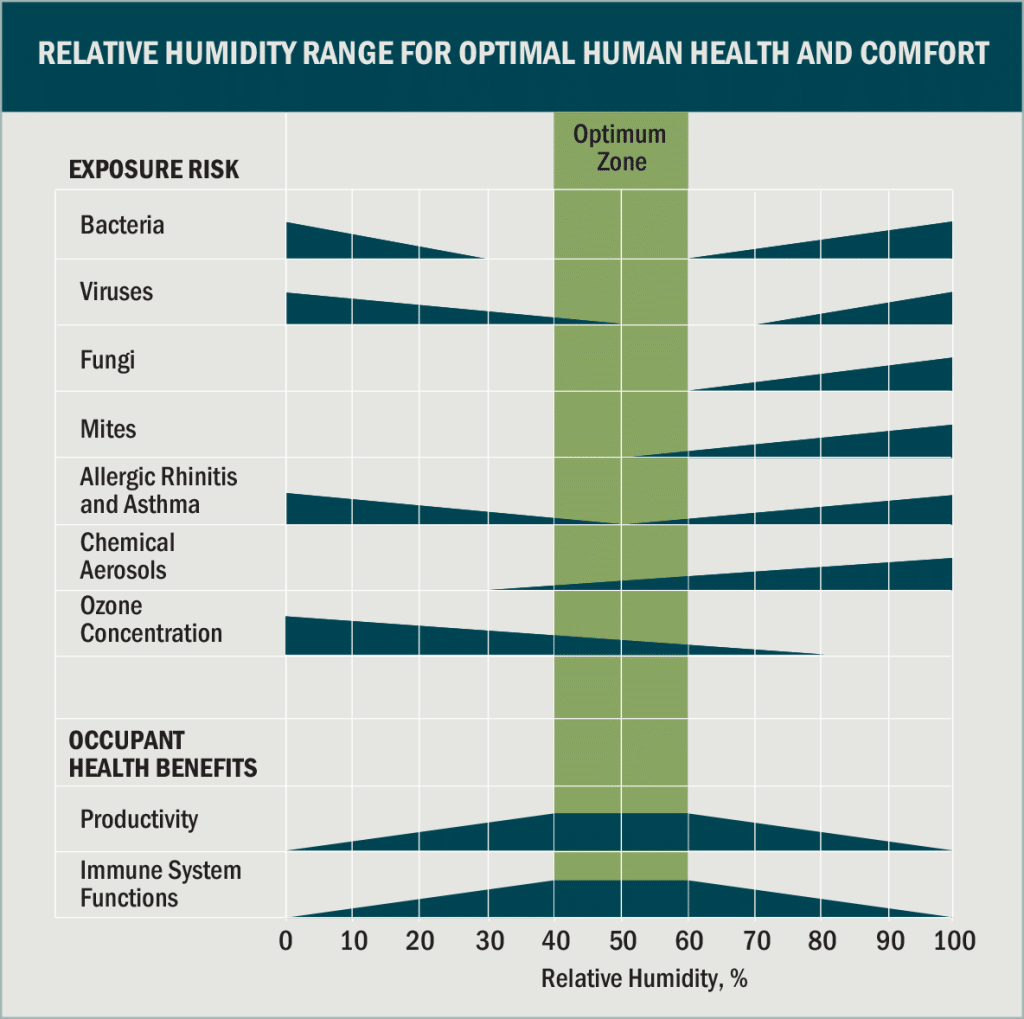
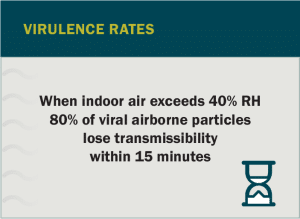
Excessively dry air can compromise certain surgical supplies, threaten patient immune system functions, and potentially increase the survival rate of airborne pathogens. For these reasons, minimum RH levels of 40 percent are generally recommended. Maintaining these levels, however, generally increases operational costs due to use of humidification equipment.
Source: ASHRAE/Taylor Healthcare Inc
Hospitals can drive down ambient air temperatures while maintaining acceptable RH levels by introducing desiccant-based dehumidification systems or supplemental chilled-water equipment such as low-temperature recirculating chillers. Although potentially more reliable, low-temperature chillers will add to the energy intensity usage of hospital operations.
Ideal Air Exchange and Air Flow
Recent studies find that the location of air returns and diffuser arrays have significant impact on how contaminants accumulate within the operating room. Room geometry, furniture location, and the position of medical staff can form air vortices that prevent microorganisms from being drawn out through the HVAC system, potentially impacting the surgical site and causing an SSI.
ASHRAE Standard 170 requires minimum of 20 air changes per hour (ACH) with two low air returns at opposite corners of the operating room. In addition, the standard requires primary supply diffusers that inject air above the patient, directing potentially contaminated air toward the floor and out the return system. ASHRAE Standard 170 states the diffuser array must cover at minimum 70 percent of the surgical table plus a 12-inch area around the table.
“Debate is underway whether increasing the number of air exchanges will result in meaningful air quality improvements.”
Source: ASHRAE
ASHRAE’s laminar diffuser coverage requirement can present one of the toughest compliance challenges. Any gaps between the diffusers, surgical lights, columns, equipment, or medical gas booms and access panels count against the allowable coverage. To demonstrate the location of potential air-flow obstacles, a Reflected Ceiling Plan (RCP) reveals whether the laminar diffuser array must be enlarged or whether the surgical equipment needs to be rearranged.
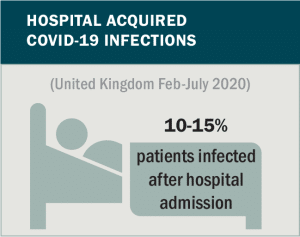
Mechanical Design Beyond COVID-19
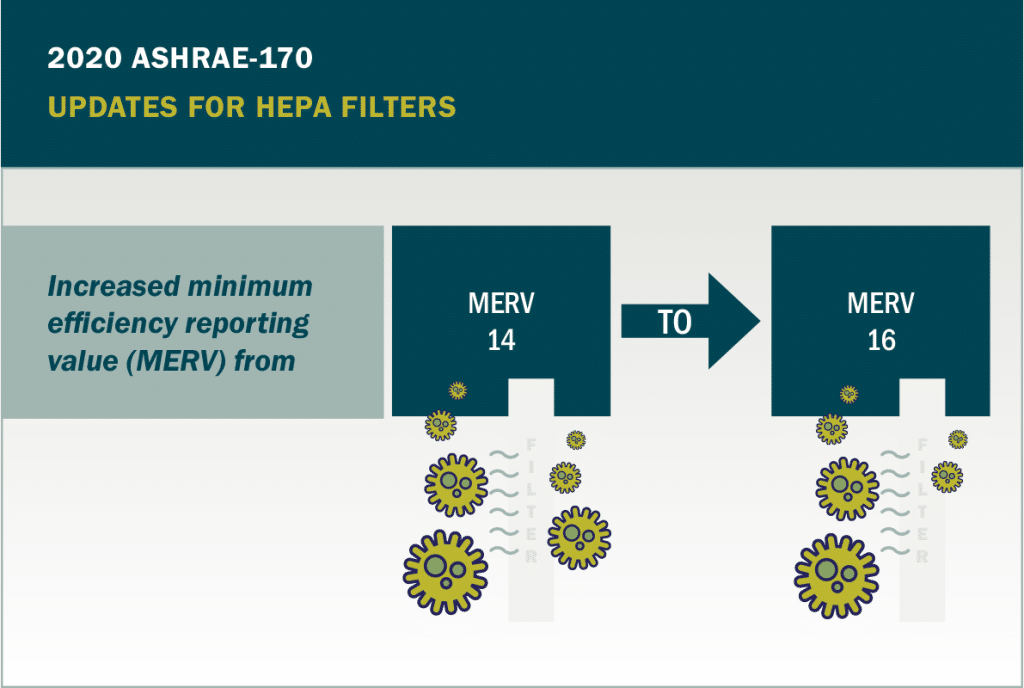
To reduce risks of COVID-19 transmissions, hospitals rapidly adapted operating room HVAC systems while ensuring minimal disruption to surgical operations. Typical upgrades included introduction of high-efficiency particulate air (HEPA) filtration systems and the incorporation of short-wavelength ultraviolet-C light (UVC) into operating room cleaning strategies or directly into the ventilation filtration systems.
Innovative COVID-19 solutions that may continue as best practice include use of surgical anterooms. Modular, negatively pressured systems have appeared adjacent to operating room entrances across the country. Combined with HEPA filters, the anterooms prove effective in limiting spread of infectious particles into surgical suite corridors.
Moving forward, how hospitals limit airborne infections within operating room environments will continue to be one of the most complex components of hospital mechanical design.
Hospitals that most effectively respond to this challenge will benefit from indoor air quality improvements, creating environments more conducive to patient care and recovery.


