Neonatal and Delivery Unit Lighting Goes from Too Bright to Just Right
This article originally appeared in Consulting-Specifying Engineer.
Newborns and birthing women thrive within softly lit, calming environments — not necessarily the best conditions for delivering medical care.
Advancements in standard care and technology options present lighting-design teams with unique challenges. Hospitals can now choose from a growing array of lighting equipment for maternal and newborn care units. Among these options, designers must find an ideal balance of intensity, color, direction, and placement for different users who often have unique — sometimes competing — lighting preferences.
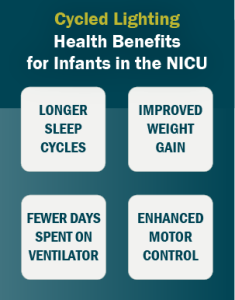
Source: Newborn and Infant Nursing Reviews
To assist hospitals in navigating these design decisions, the American National Standards Institute (ANSI)/Illuminating Engineering Society (IES) will soon be releasing RP-29-22 Recommended Practice: Lighting Hospital and Healthcare Facilities. RP-29-22 will include guidance to address the sensitive nature and complex lighting preferences of Neonatal Intensive Care Units (NICUs) and delivery units.
Lighting Design and Health Impacts
At birth, newborns emerge to find a bright, noisy hospital environment. Lighting can be especially irritating for premature babies. Pupil responses do not fully develop until around the 35th week of development. Many infants struggle to process blue light for weeks after.
Continuous bright light affects sleep cycles. Lighting levels can also undermine alertness, regulation of circadian rhythms, and feeding patterns. Overstimulation may result in greater agitation, lower blood-oxygen levels, and sub-optimal weight gain.
Lighting can have a major impact on labor and delivery as well. Birthing women thrive in relaxing environments. Dimmed lighting and changing colors can help to provide distraction and calm, potentially lowering heart rates for the woman and child, which may facilitate an unmedicated birth.
History of NICU Lighting
It took decades for NICU design to incorporate lighting choices that could support infants’ developmental preferences.
 After World War II, evolving hospital standards led many NICUs to stop isolating premature infants, instead grouping them within large rooms. Bright overhead lights stayed on 24 hours a day, enabling medical teams to tell if babies were turning pike or blue. At the time, it was one of the few ways to determine if infants needed oxygen.
After World War II, evolving hospital standards led many NICUs to stop isolating premature infants, instead grouping them within large rooms. Bright overhead lights stayed on 24 hours a day, enabling medical teams to tell if babies were turning pike or blue. At the time, it was one of the few ways to determine if infants needed oxygen.
Around the 1980s, many hospitals applied research suggesting NICU environments should mimic conditions within the womb. Dim incandescent lighting replaced harsh fluorescent bulbs.
The shift away from bright lights improved conditions for infant development. But continuous dark lighting creates new challenges:
- Sleeping newborns are often unintentionally jolted awake when lights are turned on during routine assessments.
- Insufficient daytime ambient light can disrupt infants’ sleep–wake cycle, affecting their mood and possibly diminishing weight gain.
- Constantly dim lighting can seriously disrupt daytime workers’ circadian rhythm, potentially contributing to serious health impairments.
NICUs are the only critical-care environment where indirect lighting is recommended to achieve ambient illuminance levels.
NICU and Delivery Unit Lighting Best Practices
Today, NICU design best practice is to use indirect, diffuse, and adjustable lighting. NICUs are the only critical-care environment where indirect lighting is recommended to achieve ambient illuminance levels.
 Control technologies make infinite lighting adjustments possible for NICU and delivery unit environments. Colors and intensity levels can gradually change over the course of the day, supporting the circadian system of infants, families, and care providers.
Control technologies make infinite lighting adjustments possible for NICU and delivery unit environments. Colors and intensity levels can gradually change over the course of the day, supporting the circadian system of infants, families, and care providers.
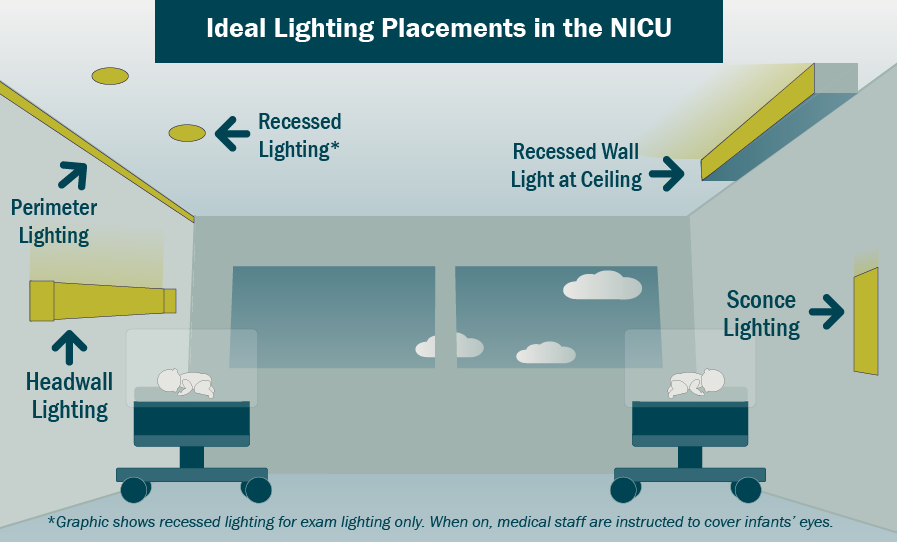
To ensure light sources do not shine directly into an infant’s sensitive eyes, light-emitting diodes (LEDs) can now be placed in seemingly every imaginable location — from the ceiling and walls to within side walls, headwalls, cabinets, and beds. Light shields or diffusers can further reduce glare.
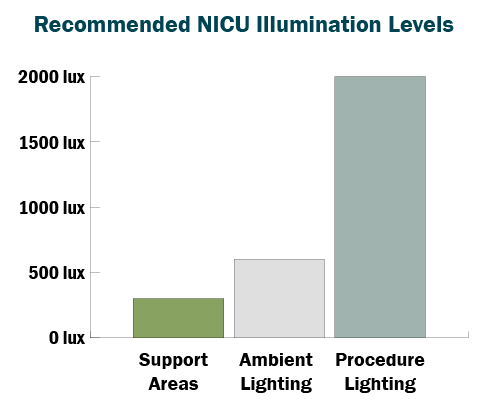
For procedural lighting, dedicated fixtures at the infant bed can aid healthcare providers’ abilities to perform assessments and critical tasks. Design standards suggest no more than 2 percent of light output should extend beyond the illumination field, ensuring task lights do not increase lighting levels for other babies located in the room.
Within delivery rooms, innovative lighting installations are going far beyond minimum standards. Multisensory rooms may twinkle like a night sky, cast patterns of a relaxing range of colors, or feature sky-and-cloud panels that give the appearance of sunlight filling the room. More units are incorporating biophilic lighting that recreates natural elements to reduce stress and that supports the hospital’s healing environment.
Updated IES Recommendations on Lighting Best Practices
Release of new IES recommendations marks a significant step forward in promoting the health and well-being of newborn infants and birthing mothers. The revised guidelines acknowledge the sensitive nature of these environments, striking a balance between the needs and preferences of different users, including infants, family members, and medical providers.
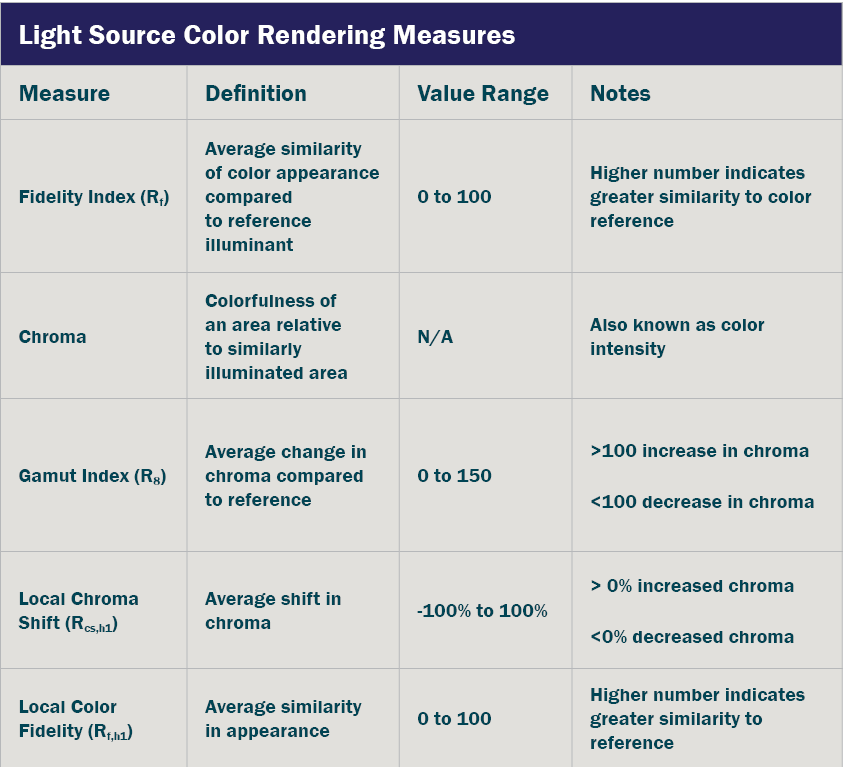
Source: ANSI/IES TM-30-18, IES Method for Evaluating Light Source Color Rendition
More specifically, the IES Healthcare Committee is revising ANSI/IES RP-29-20, Section 8.3.1.5 Nursery Units, to provide concise guidelines on color rendering metrics, lighting control application methods, and ambient lighting practices. The recommendations include a notable deviation from Facility Guidelines Institute’s Recommended Standards for Newborn ICU Design. It is now accepted that NICU color fidelity (Rf) should be greater than or equal to 80 — with a color gamut (Rg) between, or equal to, 97 and 110.
Adopting the new IES recommendations will ultimately support care delivery. When incorporated into hospital designs, restorative lighting conditions can promote newborn infants’ health, establish comforting environments for families, and support the practical needs of care providers.



